2 degrees of knee joint gonarthrosis can not only reduce a patient's motor activity, but also worsen his or her quality of life in general. The reason may not be just the pain and inability to exercise, which seems unimportant until recently.
Comparing the changes that occur between the early stages of the disease and the second stage, one begins to understand: without proper treatment, the condition will only get worse.
Causes of disease
Often, the reason for the transition of the disease to stage 2 is irresponsible attitude towards treatment and non-compliance with the doctor's recommendations on physical activity and lifestyle changes.
In joints that are already affected by the disease, blood circulation and metabolic processes are slowed down so that tissues cannot receive nutrients and oxygen without outside help. If the rejection of treatment or delay "for later", there is an acceleration of the destructive process in the joints and, as a consequence, the transformation of their mild stage disease into a more severe one.
Symptoms
Stage 2 knee gonarthrosis is characterized by the following manifestations:
- increased pain: pain attacks acquire a certain regularity (after a good night's sleep, prolonged rest periods, physical exercise);
- joint spasms, usually in the morning, that disappear after a short walk;
- the size of the knee joint increases, its relief is launched - all the bruises and physiological depression in the joint are no longer determined. In a standing position, this can appear as skin "hanging" above the knee. In the squat position, it becomes clear that one knee (affected by gonarthrosis) is much larger than the other, healthy, and has a spherical shape;
- when moving in the knee, characteristic cramps can be heard;
- Bending movements and joint elongation are very limited.
People with grade 2 gonarthrosis can rarely do without taking painkillers, as knee pain begins to interfere even at rest. This is due to a growth like spike in the bone tissue of the joint, which irritates and injures all structures of the knee.
How doctors make this diagnosis
In most cases, a patient complaining of deteriorating health has been diagnosed with gonarthrosis, and the attending physician may order an X-ray examination to assess changes in the joint.
If a doctor has reason to suspect that other diseases are associated with gonarthrosis, CT, MRI and laboratory blood tests may be recommended. This is necessary to exclude infections that can penetrate the joints through the bloodstream, and complicated gonarthrosis, with damage to the soft tissues.
Complications of the disease

If there is no irresponsible treatment or attitude towards it, class 2 gonarthrosis can quickly overcome the last "stage" and lead to the final stage, where the pain becomes a constant companion, and the joints experience changes and deformitiescannot be restored.
In addition, weak joint tissue becomes susceptible to infection, and any systemic viral or bacterial disease can cause serious complications during gonarthrosis. The most common, but no less dangerous, is an infection of the joint cavity with the formation of purulent contents, which can spread to soft tissues - muscles, skin.
Treatment
In the treatment of class 2 gonarthrosis, the focus is to relieve pain, slow down or completely stop the degenerative process in the joints, prevent complications and improve knee mobility.
Medicine
Drugs used in the treatment of grade 2 gonarthrosis are divided into the following groups:
- Anti-inflammatory drugs.This includes the latest generation of non-steroidal anti-inflammatory drugs (NSAIDs), which eliminate the inflammatory process in the joints and, as a consequence, reduce pain.
- Chondroprotectors.This group of drugs helps protect cartilage tissue from further destruction and enhances the regrowth process in it.
- A preparation of hyaluronic acid,which is an analog of the natural lubrication of the inner surface of the joint. By reducing friction on the knee joint, these drugs prevent cartilage wear. In some cases, intra-articular injections of hyaluronic acid are indicated (for example, with very poor blood circulation in the joints, which prevents other forms of medication from reaching the affected tissue).
- Help.These include vitamin preparations, immunostimulants, bioactive extracts from plants (aloe vera, echinacea, etc. ), which are designed to increase blood circulation in the articular tissue and thus speed up metabolic processes in it.
Physiotherapy, massage, exercise therapy

Treatment methods such as physiotherapy therapy, massage and exercise can be considered as assistants in the treatment of grade 2 gonarthrosis and are rarely used as independent treatment methods.
Physiotherapy (UHF, phonophoresis, ultrasound therapy, magnetotherapy) is used to improve blood circulation in the joints and stimulate the recovery process in them.
One of the most effective physiotherapeutic procedures for the treatment of arthrosis is MLS laser therapy with the ability to regulate the power of laser radiation. This therapy uses a continuous and pulsating wavelength, as deep penetration into the tissue and significant clinical effects are achieved. Laser MLS treats all diseases of the joints, osteochondrosis, hernias and other diseases of the musculoskeletal system.
Massage is recommended in a 10-15 session course, one session per day or per day. By improving blood circulation in the joints, massage normalizes the metabolic processes in it and gives a more effective drug effect on diseased tissues.
In the diagnosis of stage 2 knee joint arthrosis, massage with the use of drugs (chondroprotectors, anti-inflammatory or irritating ointments, refrigerants and anesthetic external agents) is often prescribed. factor.
The physiotherapy training complex is assigned to the attending physician after evaluating the effectiveness of the drug treatment, and is selected taking into account the individual characteristics of the disease course and the general health of the patient.
Lifestyle correction
Lifestyle correction is one of the most important conditions for effective treatment. With 2nd degree gonarthrosis, you must adhere to the following rules:
- Reduces load on diseased joints.For this, an orthopedic crutch is used, which allows you to distribute the load during such movements until the knee joint is minimally involved. It is important to choose a cane that fits your height - necessarily from the wrist to the floor as you stand.
- Diet.For this disease, it is recommended to reduce the consumption of foods that contain animal protein (eggs, meat, fish, whole milk), carbohydrates (baked goods, sweets) and foods and beverages that contain synthetic flavors, sweeteners, preservatives.
- Weight. Obesity is one of the risk factors that increases the likelihood of metabolic disorders in all tissues, including joint tissues. Also, being overweight is an unnecessary stress on the joints.
Surgical Treatment
Surgical treatment can be divided into two types: arthroscopy and endoprosthetics.
Each operation has its own list of indications for which intervention will be most effective.
Arthroscopy

Arthroscopy is a method of low trauma surgery in which surgery is performed using miniature lighting, surgical instruments and video inserted into the joint cavity through a small puncture.
Reading:
- the presence of bone neoplasms (osteophytes) that inhibit joint movement;
- joint tissue defects, which can be repaired without large-scale surgical intervention;
- needs chondroplasty, which can significantly slow the progression of the disease and restore joint mobility.
Contraindications to arthroscopy are acute infectious diseases, blood clotting disorders and slight movement in the joints - the inability to lengthen or flex the joints completely does not allow the surgeon to perform the necessary manipulations.
Endoprosthetics
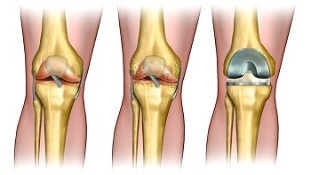
Endoprosthetics - the replacement of artificial knee joints made of durable and hypoallergenic materials, whose structure is similar to natural bone tissue.
Over time, the prosthesis takes over all "native" joint functions and allows you to return to normal life.
Reading:
- no effect after long conservative treatment;
- rapid disease progression;
- changes in the joints significantly interfere with the patient's motor activity, causing severe and frequent pain and / or causing the risk of disability.
Among the absolute contraindications is only systemic diseases that make surgical manipulation impossible.
The treating physician considers the risks and benefits of surgical treatment, and, based on the conclusions reached, decides on the need for surgery or to continue conservative treatment.

















































